Peripheral arterial disease
Puts you at risk of
heart attack or stroke
Pain or cramping in your legs — even if it's mild — can be a sign of peripheral arterial disease (PAD). This disease in your arteries (usually your legs) can cause blood flow to be reduced, which can lead to more serious or life-threatening complications. That's why it's important to talk to your doctor if you think you have PAD, so you can work to reduce your risk of heart attack, stroke, or amputation.
- Are you at risk for PAD? Use the PAD
Risk Assessment tool to find out. PAD Risk Assessment
PAD Risk Assessment
 Not an actual patient
Not an actual patient

Cause of peripheral arterial disease
If you have peripheral arterial disease (PAD), arteries in your body (usually your legs) are narrowed or blocked, which can reduce blood flow and may cause pain.
These blockages in your legs can be a sign that there are also blockages in the arteries supplying your heart and brain with blood. This can lead to heart attack and stroke.
PAD can also lead to critical limb ischemia: a condition where injuries or infections on your feet or legs don’t heal and get worse. This can result in gangrene (tissue death) and sometimes may require amputation of the affected limb.
Symptoms of peripheral
arterial disease

Many people don’t recognize the symptoms of peripheral arterial disease (PAD) because they are similar to what they might associate with aging, arthritis, or diabetic neuropathy. As a result, people may not mention their pain to their doctor. If you have any of the symptoms of PAD listed below, talk to your doctor.
- Painful cramping in the hips, thighs, or calves when walking, climbing stairs, or exercising (known as intermittent claudication)
- Leg pain that does not go away when you stop exercising
- Foot or toe wounds that won’t heal or heal very slowly
- Gangrene, or dead tissue
- A noticeable decrease in the temperature of your lower leg or foot, particularly compared to the other leg or to the rest of your body
- Poor toenail or leg hair growth
- Erectile dysfunction, especially in men with diabetes
 Not an actual patient
Not an actual patient

Risk factors for peripheral arterial disease
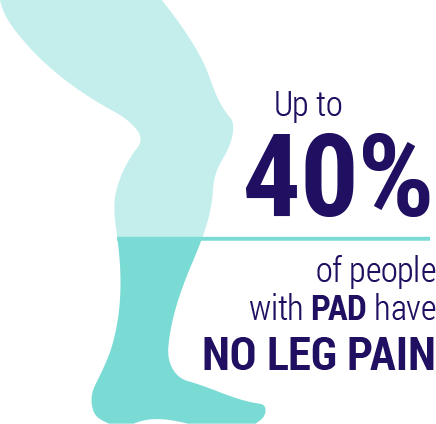
Up to 40% of people with peripheral arterial disease (PAD) have no leg pain at all. Even if you don’t have any of the symptoms of PAD listed above, talk to your doctor if you have any of the risk factors for PAD listed below.
- Diabetes
- Smoking
- High blood pressure
- High cholesterol
- Overweight and obesity
- Lack of regular exercise
- Age (over 60)
- Family history of PAD
- Family history of heart disease

Treatment for peripheral arterial disease
Possible treatments for peripheral arterial disease (PAD) involve lifestyle changes, medications, or medical procedures.
These options aim to improve symptoms, slow progression of the disease, or lower the risk of heart attack or stroke.
Lifestyle Changes
- Quitting smoking
- Supervised exercise program
- Eating a heart-healthy diet
Medications
- Antiplatelet therapies like ZONTIVITY® (vorapaxar), aspirin, and clopidogrel (Plavix®) help prevent blood clots that can lead to events like heart attack and stroke
- Statins are cholesterol-lowering medications that help reduce risk of heart attack and stroke
- High blood pressure medications may be used to lower your blood pressure
- Medication to control your blood sugar may be used to control your glucose levels if you have diabetes
- Symptom-relief medications, like cilostazol (Pletal®) and pentoxifylline (Trental®) are sometimes used to increase blood flow to the legs and improve leg pain
Medical Procedures
- Angioplasty is a procedure that uses a small, hollow tube (catheter) to place a small balloon in the affected artery. The balloon is inflated to widen the artery, move the blockage out of the way, and increase blood flow. A mesh framework, or stent, is also sometimes inserted to help keep the artery open
- Bypass surgery involves taking a blood vessel from another part of the body or using a synthetic vessel to allow the blood to flow around the blockage
- Thrombolytic therapy is when a doctor injects a medication into a blocked artery at the point of a blood clot to break it up
Diagnosing Peripheral Arterial Disease
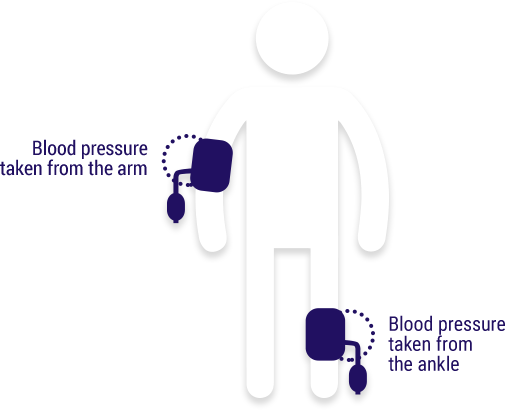
Talk to your doctor about the ankle-brachial index (ABI): a painless exam that compares the blood pressure in your feet to the blood pressure in your arms to see how well your blood is flowing. The ABI can be done by your doctor right in the office as part of a routine visit.
Indication
ZONTIVITY is a prescription medicine used to treat people who have
- had a heart attack or
- reduced blood flow in their legs (peripheral arterial disease).
ZONTIVITY is used with aspirin and/or clopidogrel to lower your chance of having another serious problem with your heart or blood vessels, such as heart attack, stroke, or death
Important Safety Information
WHAT IS THE MOST IMPORTANT INFORMATION I SHOULD KNOW ABOUT ZONTIVITY?
ZONTIVITY is used to lower your chance of having another serious problem with your heart or blood vessels, but ZONTIVITY (and similar drugs) can cause bleeding that can be serious and lead to death.
Call your doctor right away if you have any of these signs or symptoms of bleeding while taking ZONTIVITY:
- bleeding that is severe or that you cannot control
- pink, red, or brown urine
- vomiting blood or your vomit looks like "coffee grounds"
- red or black stools (looks like tar)
- coughing up blood or blood clots.
While you take ZONTIVITY and for about 4 weeks after your treatment with ZONTIVITY is stopped:
- you may bruise and bleed more easily (nose bleeds may be common)
- it will take longer than usual for any bleeding to stop.
Do not take ZONTIVITY if you:
- have had a stroke or "mini stroke" (also known as transient ischemic attack or TIA)
- have had bleeding in your brain
- currently have unusual bleeding, such as bleeding in your head, stomach or intestines (an ulcer).
If you have a stroke, TIA, or bleeding in your brain while taking ZONTIVITY your doctor should stop your treatment with ZONTIVITY. Follow your doctor's instructions about stopping ZONTIVITY.
Take ZONTIVITY exactly as prescribed by your doctor. Do not stop taking ZONTIVITY without first talking to the doctor who prescribed it for you.
Before you take ZONTIVITY, tell your doctor if you:
- have had bleeding problems or history of stomach ulcers
- have had a stroke or "mini-stroke" (also known as transient ischemic attack or TIA)
- have had bleeding (hemorrhage) in your brain
- have had any recent serious injury or surgery
- plan to have surgery or a dental procedure
- have kidney problems or severe liver problems
- are pregnant or plan to become pregnant. It is not known if ZONTIVITY will harm your unborn baby.
- are breastfeeding or plan to breastfeed. It is not known if ZONTIVITY passes into your breast milk. You and your doctor should decide if you will take ZONTIVITY or breastfeed. You should not do both.
Tell all of your doctors and dentists that you are taking ZONTIVITY with aspirin, with clopidogrel (Plavix®), or with aspirin and clopidogrel. They should talk to the doctor who prescribed ZONTIVITY for you before you have any surgery or dental procedure.
The possible side effects of ZONTIVITY include:
- Bleeding that can be serious and lead to death (see above)
- Anemia (low level of red blood cells)
- Depression
- Rash
These are not all the possible side effects of ZONTIVITY.
Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, dietary or herbal supplements. Taking ZONTIVITY with certain other medicines may increase your risk of bleeding and may affect how ZONTIVITY works.
The risk information provided here is not comprehensive. To learn more, talk about ZONTIVITY with your pharmacist or other health care providers. The product information can be found at www.zontivity.com or call at 1-800-988-6115.
Call your doctor for medical advice about side effects. You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088.
Please click here for Medication Guide, including Important Warning about bleeding risk.
Indication
ZONTIVITY is a prescription medicine used to treat people who have
- had a heart attack or
- reduced blood flow in their legs (peripheral arterial disease).
ZONTIVITY is used with aspirin and/or clopidogrel to lower your chance of having another serious problem with your heart or blood vessels, such as heart attack, stroke, or death
Important Safety Information
WHAT IS THE MOST IMPORTANT INFORMATION I SHOULD KNOW ABOUT ZONTIVITY?
ZONTIVITY is used to lower your chance of having another serious problem with your heart or blood vessels, but ZONTIVITY (and similar drugs) can cause bleeding that can be serious and lead to death.
Call your doctor right away if you have any of these signs or symptoms of bleeding while taking ZONTIVITY:
- bleeding that is severe or that you cannot control
- pink, red, or brown urine
- vomiting blood or your vomit looks like "coffee grounds"
- red or black stools (looks like tar)
- coughing up blood or blood clots.
While you take ZONTIVITY and for about 4 weeks after your treatment with ZONTIVITY is stopped:
- you may bruise and bleed more easily (nose bleeds may be common)
- it will take longer than usual for any bleeding to stop.
Do not take ZONTIVITY if you:
- have had a stroke or "mini stroke" (also known as transient ischemic attack or TIA)
- have had bleeding in your brain
- currently have unusual bleeding, such as bleeding in your head, stomach or intestines (an ulcer).
If you have a stroke, TIA, or bleeding in your brain while taking ZONTIVITY your doctor should stop your treatment with ZONTIVITY. Follow your doctor's instructions about stopping ZONTIVITY.
Take ZONTIVITY exactly as prescribed by your doctor. Do not stop taking ZONTIVITY without first talking to the doctor who prescribed it for you.
Before you take ZONTIVITY, tell your doctor if you:
- have had bleeding problems or history of stomach ulcers
- have had a stroke or "mini-stroke" (also known as transient ischemic attack or TIA)
- have had bleeding (hemorrhage) in your brain
- have had any recent serious injury or surgery
- plan to have surgery or a dental procedure
- have kidney problems or severe liver problems
- are pregnant or plan to become pregnant. It is not known if ZONTIVITY will harm your unborn baby.
- are breastfeeding or plan to breastfeed. It is not known if ZONTIVITY passes into your breast milk. You and your doctor should decide if you will take ZONTIVITY or breastfeed. You should not do both.
Tell all of your doctors and dentists that you are taking ZONTIVITY with aspirin, with clopidogrel (Plavix®), or with aspirin and clopidogrel. They should talk to the doctor who prescribed ZONTIVITY for you before you have any surgery or dental procedure.
The possible side effects of ZONTIVITY include:
- Bleeding that can be serious and lead to death (see above)
- Anemia (low level of red blood cells)
- Depression
- Rash
These are not all the possible side effects of ZONTIVITY.
Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, dietary or herbal supplements. Taking ZONTIVITY with certain other medicines may increase your risk of bleeding and may affect how ZONTIVITY works.
The risk information provided here is not comprehensive. To learn more, talk about ZONTIVITY with your pharmacist or other health care providers. The product information can be found at www.zontivity.com or call at 1-800-988-6115.
Call your doctor for medical advice about side effects. You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088.
Please click here for Medication Guide, including Important Warning about bleeding risk.
